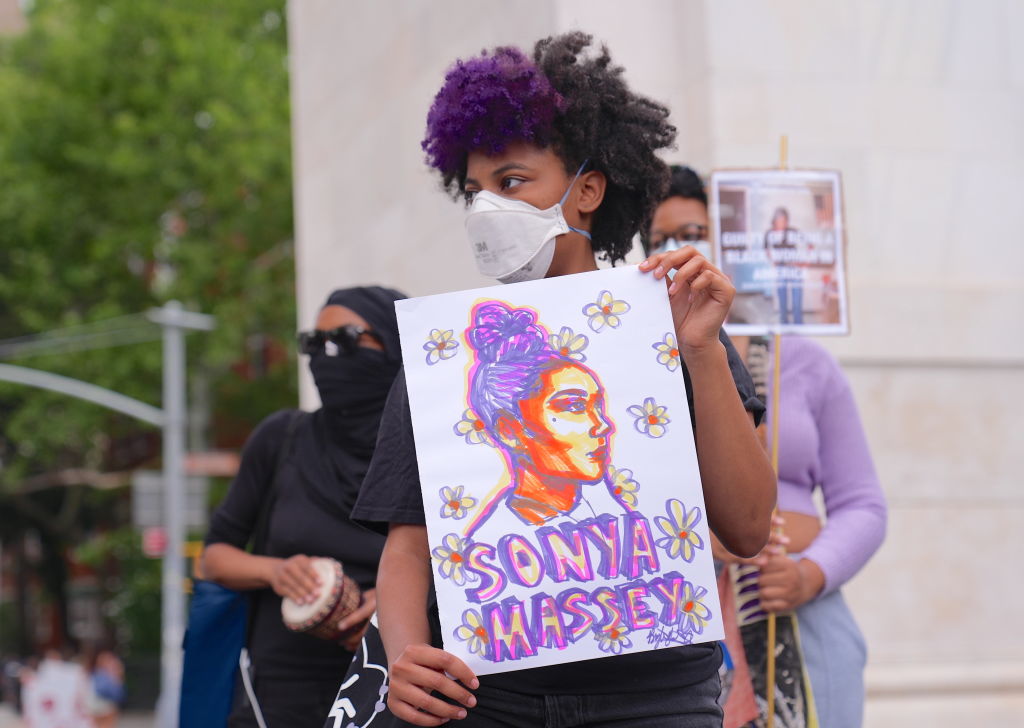
Sonya Massey was Black and had a mental illness: two big triggers for police brutality in the US
On July 6, 2024, Sonya Massey, 36, called 911 to report a potential intruder at her home in Springfield, Illinois. Roughly 30 minutes after two policemen arrived at her house, Massey lay dying on her kitchen floor, shot in the head by one of the officers.
The bodycam video of the shooter’s partner was recently released and so the whole world watched, once again, how a defenseless black person was killed by an armed police officer who considered her a threat for no good reason.
While the outrage of the American people has been understandably focused on the fact that Massey was Black, she had also been diagnosed with paranoid schizophrenia, according to her family, a factor that already made her way more vulnerable during an encounter with armed police.
People with a severe mental illness are 16 times more likely to be killed during a police encounter than other civilians approached or stopped by law enforcement, according to the Treatment Advocacy Center.
This, according to a Washington Post database of fatal U.S. shootings by on-duty police officers. Since 2015, when The Post launched its database, police had fatally shot more than 1,400 people with mental illnesses. Now Massey could be added to that list.
Almost half of the people who die at the hands of police have some kind of disability, according to a report published by the Ruderman Family Foundation, a disability organization.
Angela Kimball, national director of advocacy and public policy for the National Alliance on Mental Illness, said she believes the numbers are so high because people in mental health crises do not always respond in ways officers want them to.
Haben Girma, a lawyer and activist who has a hearing and a visual impairment, told TIME: “Someone might be yelling for me to do something and I don’t hear. And then they assume that I’m a threat.”
Coverage of police brutality cases have been hugely focused on race, and while that plays a big role in police brutality in the US, that lens can also obscure how disability and mental health problems also factor into police interactions.
Another example is the shooting of LaQuan McDonald in 2014, a black teenager who was killed by the police while acting erratically and holding a knife. Prosecutors charged an officer with first-degree murder, noting McDonald did not pose a lethal threat to the officers who had surrounded him.
When the video of the shooting was released, it sparked the resignation of Chicago’s police chief and a national debate over race and policing. There was far less focus, however, on McDonald’s health.
According to a later investigation by the Chicago Tribune, McDonald suffered from PTSD and “complex mental health problems.”
Black people are more likely than white people to have chronic health conditions, more likely to struggle when accessing mental-health care and less likely to receive formal diagnoses for a range of disabilities, according to the CDC.
Have lower incomes than white Americans and live in less safe neighborhoods. These factors contribute to worse mental health outcomes.
A 2016 report from the Police Executive Research Forum found that nationwide, police academies spend a median of 58 hours on firearm training and just eight hours on de-escalation or crisis intervention.
Crisis-intervention training, which is designed to help officers safely and calmly interact with people with disabilities and de-escalate confrontations with the mentally ill.
Arc, one of the United States’ largest disability-rights organizations has a program to teach law-enforcement officers, lawyers, victim-services providers and other criminal-justice professionals how to identify, interact with and accommodate people with disabilities.
Hamilton Police Service's new Mental Health Crisis Response Training Program uses virtual reality to help teach police officers to recognize the signs of a mental health crisis and improve how they de-escalate situations.
Nevertheless, sometimes police interventions can make health crises worse. For instance, there was a case of a woman in Tempe, Arizona who called the police because her 29-year-old son, who had bipolar disorder and schizophrenia, was experiencing a manic episode.
The woman needed help getting him to a mental health facility. But when police showed up at her apartment with riot shields and rifles, they all panicked, including the son, the officers were yelling, and the situation quickly escalated.
Tempe Police Chief Sylvia Moir told TIME that we have to first consider this question: “Is the police the right societal actor to be inserted into this space and into this societal issue?”
CAHOOTS (Crisis Assistance Helping Out on the Streets), is a program that reroutes 911 and non-emergency calls relating to mental health, substance use or homelessness to a team of medics and crisis-care workers. Those teams respond to such calls instead of the police.
Social stigma leads to a perception of people with a mental illness as being violent and dangerous. Nevertheless, according to the American Psychiatric Association, most people with mental illness are not violent, and using law enforcement as a blunt instrument contributes to the stigma that they are.
In fact, according to the World Health Organization (WHO) people with a mental illness are much more likely to be victims of a crime than to commit one, as they are a vulnerable group of society.
Sean Grayson, the 30-year-old officer who killed Massey, who has since been fired from the agency, was indicted by a grand jury last week on three counts of first-degree murder and one count each of aggravated battery with a firearm and official misconduct, CNN reported.
More for you
Top Stories